 Researchers have taken an important step forward in the ongoing fight against HIV. A recent Phase 1 trial found that an mRNA-based vaccine can trigger an antibody response in as many as 80% of participants. Inspired by COVID-19 vaccine advances, this innovative approach uses mRNA to deliver the stable ‘stem’ protein of HIV—a part of the virus that remains mostly unchanged even as it mutates.
Researchers have taken an important step forward in the ongoing fight against HIV. A recent Phase 1 trial found that an mRNA-based vaccine can trigger an antibody response in as many as 80% of participants. Inspired by COVID-19 vaccine advances, this innovative approach uses mRNA to deliver the stable ‘stem’ protein of HIV—a part of the virus that remains mostly unchanged even as it mutates.
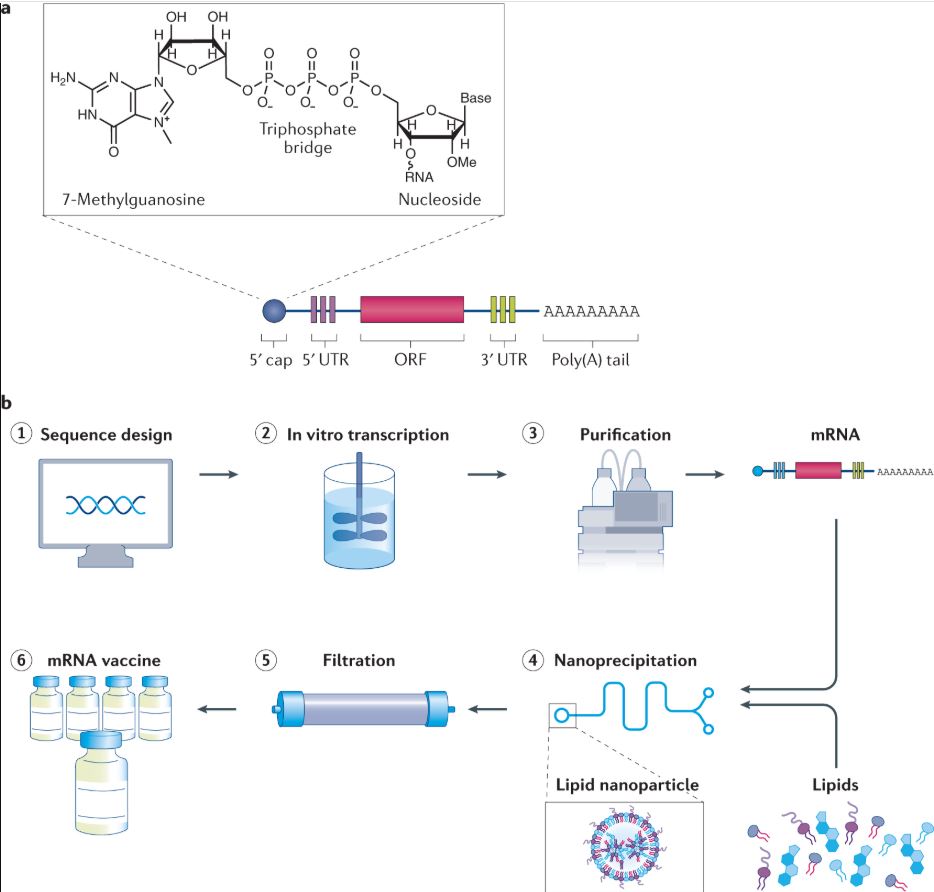
Once the vaccine is administered, your cells start producing this protein, effectively signalling the immune system to prepare for a possible threat. Animal experiments in rabbits and monkeys were very promising, and early human trials have confirmed that the vaccine is generally safe, with some participants experiencing mild, persistent rashes.
Led by William Schief at the Scripps Research Institute, the study highlighted the potential of using a membrane-bound version of the protein. In these trials, the membrane-bound form successfully generated antibodies in 80% of recipients, while the soluble form managed to do so in only 4% of cases. As noted by Sharon Lewin from the Peter Doherty Institute for Infection and Immunity, “The difference is pretty striking.”
Since its discovery in the 1980s – when unusual cases of pneumonia and cancer in young men first hinted at a new threat – HIV has puzzled scientists. Even though antiviral drugs have transformed HIV from a deadly illness to a manageable condition, a preventative vaccine has remained an elusive goal, largely due to the virus’s rapid mutation and the high cost of current treatments.
In 2025, there was also a major development with the approval of an HIV-prevention drug that requires only bi-annual injections, offering protection for about six months even in high-risk regions. Other genetic strategies, like stem cell transplants, have shown promise in reducing susceptibility to HIV, though they remain complex and expensive.
This mRNA vaccine approach represents a refreshing alternative to conventional methods. By encoding virus-specific proteins directly into cells, the vaccine effectively ‘trains’ the immune system to recognise and combat HIV. Prior efforts have often focused on the more variable ‘Env’ protein, but this new strategy targets both soluble and membrane-bound forms, resulting in a significantly stronger immune response.
Animal tests were impressive. Rabbits maintained antibody levels for up to 24 weeks, and in monkeys, there was a noticeable reduction in HIV levels over 26 weeks. These encouraging results paved the way for human trials, which involved 108 participants aged between 18 and 55 from several U.S. sites.
The main focus during the human trials was to assess both safety and the antibody response. The membrane-bound protein consistently outperformed its soluble counterpart, with an 80% success rate. Although a few volunteers experienced minor side effects, such as persistent rashes, these issues are seen as a modest setback when weighed against the vaccine’s potential impact for the more than 41 million people living with HIV worldwide.
If you’ve ever followed HIV research, you’ll appreciate the cautious optimism these findings inspire. While challenges remain, this new approach offers a practical pathway for future prevention strategies. As further trials are planned, the lessons learned here could be essential for refining not only HIV vaccines but also approaches to other complex viruses.
The study gives us a renewed sense of progress and emphasises that even small advances can build towards a major breakthrough. For those looking to stay informed, this research could be the stepping stone to a more comprehensive and effective HIV prevention programme.